Working-age Canadians who live through a major depressive episode go on to experience a loss in earnings that persists for at least a decade, a study conducted by an Institute for Work & Health (IWH) researcher has found.
Drawing on tax files and a series of nationally representative health surveys conducted by Statistics Canada, the study found Canadian men who experienced a depressive episode in a given year earned $115,000 less, on average, over the next 10 years than men who had not experienced depression in the same year. Women who experienced a depressive episode earned $71,000 less, on average, than those who had not over the same time period.
The study, published in April 2021 in the Journal of Affective Disorders (doi:10.1016/j.jad.2021.02.019), found that the earnings drop took place immediately during the year that the depressive episode occurred. The result was a loss of about $5,000 for men and $4,500 for women in the first year. These workers did not see their earnings recover during the study’s 10-year follow-up. Instead, the earnings of the men fell behind by another $730 the year after depression was reported, growing to a further $1,800 behind each year by the end of the decade. The earnings of the women fell behind by another $360 a year with each passing year over the next decade.
“This drop in earnings in the first year surrounding depression may be due to people being less productive at work, taking time off work for a disability leave, or leaving a job altogether,” says IWH Research Associate Kathleen Dobson, who led this study as part of her doctoral thesis at the University of Toronto’s Dalla Lana School of Public Health.
The lower earnings over the long term are harder to explain. “It may be that employers are more reluctant to promote or offer pay increases to people they see as less productive,” says Dobson. “It may be that people with depression stay in lower paying jobs, potentially to keep their health benefits, or don’t switch to higher paying jobs for fear of the work stress they may entail. Or perhaps people don’t have stable employment over the decade following a depressive episode,” she says. “These are avenues that we definitely need to explore in future research.”
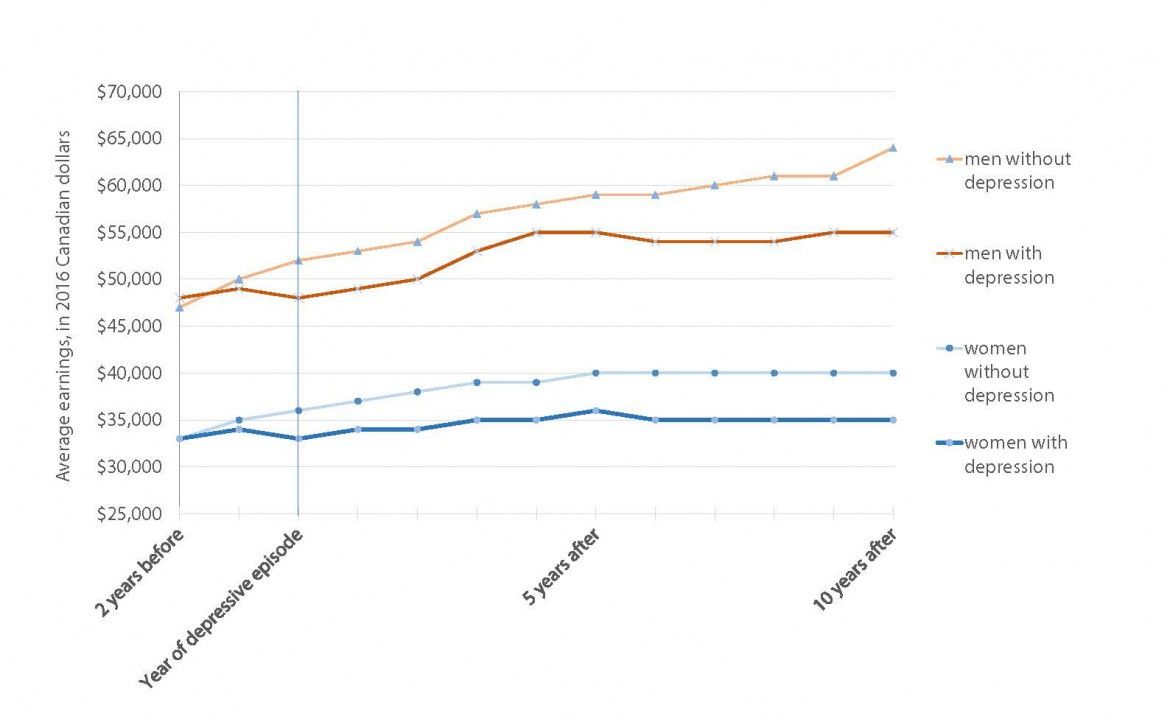
10-year follow-up
The study drew on nearly 800,000 records of people who took part in Statistics Canada’s Canadian Community Health Survey (CCHS) during the period 2003 to 2014. The CCHS, which went out every two years until 2007 and then annually until 2014 to a nationally representative sample of Canadians, covered in detail topics related to health, public health, lifestyle and health behaviours.
The study zeroed in on survey participants who were 18 to 54 years old when they took part in the survey and who had answered questions about depressive symptoms. Using only the survey data of people who agreed to have their tax filings linked to the CCHS responses, and who had earned at least $5,000 the year before the episode of depression, the study ended up with a sample of 85,000.
Previous studies on the impact of depression on people’s earnings have been inconsistent in their results. Some found no negative effect on earnings, while others found a link between depression and lower earnings in the range of $2,000 to $5,000.
The differing methods used in previous studies may account for the varied findings. The studies that found no impact on income tended to use shorter time frames or to focus on younger adults—that is, on “people who may not have spent enough time in the workforce for a difference in earnings to be visible,” says Dobson.
As well, most previous studies failed to account for the many factors that result in systematic differences between people with and without depression. “We know from other studies that people with depression are more likely to have certain characteristics. They’re more likely to be women, to not be married, to have a chronic condition, and so on. These systematic differences make it difficult to ensure that, when we see an effect on earnings, we’re seeing the effect of depression and nothing else,” says Dobson.
Dobson’s study addressed these challenges by following workers from a wide age range (18 to 54) and over a long period of time (10 years). She also used a complex study design called “propensity score matching” to ensure she was seeing the effect of depression on earnings. This method involved pairing each individual survey respondent who had depression with another survey respondent who was like them in almost every way except for the depression.
The pairs were matched on gender, year they took part in the health survey, province, age, pregnancy status, and a range of sociodemographic and health factors (including rural versus urban residency, race, immigrant status, economic household type, marital status, education level, number of young children, and number and type of diagnosed chronic conditions). Notably, they were also matched on earnings two years before the depressive episodes.
“Essentially, we created pairs that were as similar to each other as possible. For example, a married, 39-year-old racial-minority man with two kids under the age of six, who lived in small-town Ontario, had a college degree, had no chronic conditions and was earning $62,000 a year would be matched with a man who could be described in very much the same way,” says Dobson. “As a result of that work, when we saw the differences in earnings after one of the pair had a depressive episode, we were confident it was due to the depressive episode.”
This study is the second of three studies that make up Dobson’s thesis. In the first study, published by Statistics Canada in Health Reports, she estimated the prevalence of depression among working-age Canadians between 2000 and 2016—5.4 per cent among workers, 11.7 per cent among unemployed Canadians, and 9.8 per cent among those not in the labour force. An upcoming study will build on this study about earnings loss to examine the economic impact when individuals experience more than one episode of depression.