About 35 to 40 per cent of emergency department visits for the treatment of work-related injuries or illnesses in Ontario don’t show up as work-related injury claims in the records of the province’s workers’ compensation agency.
That’s according to a study conducted by an Institute for Work & Health (IWH) team, based on a data linkage between Ontario’s emergency department records and Workplace Safety and Insurance Board (WSIB) claims data.
The extent of work injury under-reporting
that can be inferred by this discrepancy may be startling,
said study lead Dr. Cameron Mustard in an IWH Speaker Series presentation in June 2021.
But based on work that the Institute has done over more than two decades, we are comfortable with that estimate,
he added. Somewhere between 40 and 60 per cent of potentially compensable conditions are typically not reported to provincial compensation authorities in Canada.
The discrepancy represents about 50,000 cases a year of work-related injuries and illnesses treated in Ontario’s emergency departments that do not correspond to a claim in WSIB records, noted Mustard, IWH president and senior scientist before his retirement in January 2022.
A portion of these cases may involve workers who are not covered by the WSIB. About 25 per cent of Ontario workers do not work for a WSIB-insured employer, and about one-third of that 25 per cent are self-employed workers, some of whom work in either moderate- or high-hazard sectors,
added Mustard.
For the remainder, more research would be useful to further explore the reasons why incidents of work-related injury or illness don’t lead to a WSIB claim, he said. This includes finding out why about 15 per cent of claims that are initially registered with the WSIB are abandoned—i.e. not followed through with the submission of the worker report.
One idea we’re attracted to is using the health-care professionals’ reports received by the WSIB that are not followed up subsequently by employer and worker reports,
said Mustard. We could use the information on the health-care providers’ forms to contact workers and ask them what their experience was, and why they chose not to register a claim with the WSIB.
Data covers 14-year span
The data linkage work by Mustard and his team covers a 14-year period from 2004 to 2017. The team began with the records of all emergency department visits in Ontario. Since 2000, hospitals in the province have been required to report all emergency visits to the National Ambulatory Care Reporting System (NACRS), held by the Canadian Institute for Health Information. When patients arrive in the emergency department, health-care providers assess aspects of their history, including whether their injury or illness arose from work. This determination of work-relatedness does not depend on whether a compensation claim is later submitted or approved.
During the study period, the team found 1.9 million emergency visits attributed to work-related causes that involved a patient aged 15 to 65. For each of these visits, the team looked for a matching WSIB claim, based on gender, birth date, postal code, date of injury and date of the emergency room visit.
Overall, about 64 per cent of workers who received treatment in an Ontario emergency department had a linked claim with the WSIB. The proportion of linked records was similar for men and women. It varied slightly across the five geographic regions of the province, ranging from 58 per cent in metropolitan Toronto to 67 per cent in western Ontario. No major difference was found across types of injuries. For example, the linkage rate for superficial injuries (66.1 per cent) was relatively close to that of open wounds (64.7 per cent) or knee injuries (70.2 per cent).
Notable shift in reporting patterns
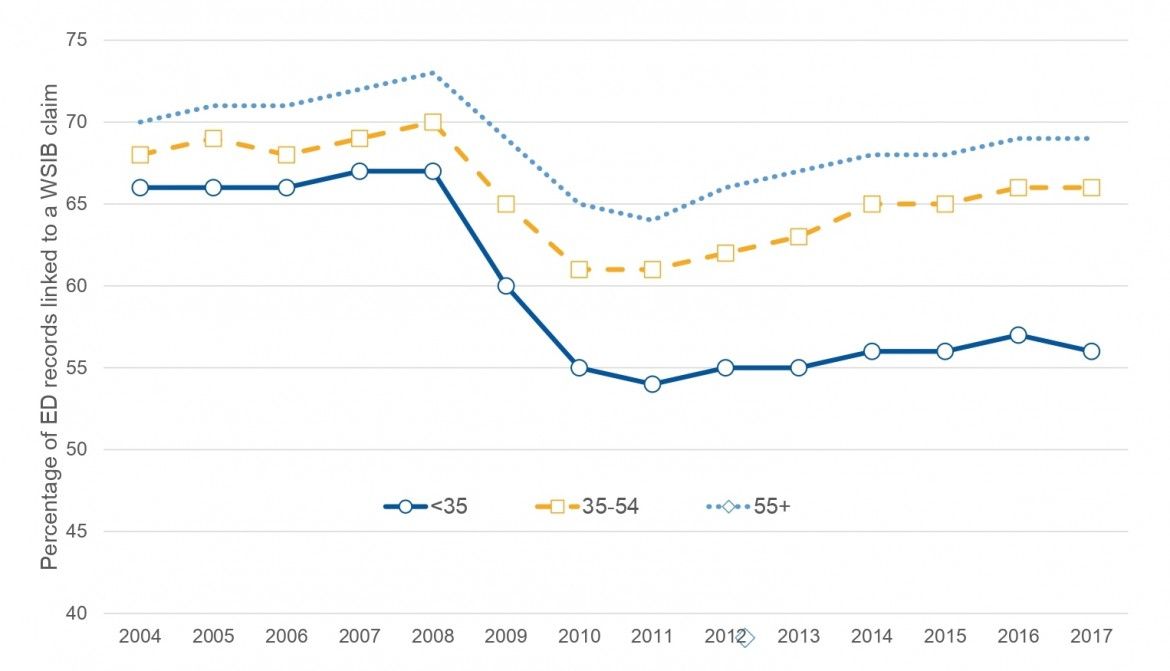
However, the team found a notable shift in reporting patterns during the 14-year time span—one that calls out for further exploration, said Mustard. In the years around the 2008-2009 global financial crisis, the proportion of work-related injuries or illnesses treated in emergency rooms that could be linked to a WSIB claim fell abruptly—from 69 per cent in 2007-08 to 59 per cent in 2011. That drop in the linkage rate was most evident among younger workers (see graphic below). In the period that followed, from 2012 to 2017, the linkage rate recovered slightly—and mainly among older age groups. The overall decline in linkage rate represented about 81,200 illnesses and injuries that would have been found in WSIB records from 2007 to 2010 had the 2007 rate of linkage been maintained.
This change in linkage rate cannot be explained entirely as an effect of an economic slowdown on work-injury rates, Mustard noted. As explained elsewhere, a decline in work injury during an economic downturn is not unusual. Indeed, from 2007 to 2009, Mustard’s research team found emergency department visits fell by 20 per cent and WSIB claims fell by 25 per cent. But these trend lines moved in parallel with each other, both rising modestly after the global financial crisis.
The drop in linkage rate after the financial crisis was caused by something else, Mustard noted. Before the global financial crisis, there was only a minor difference across age groups in the percentage of emergency department records that could be matched to a parallel compensation claim. When the global financial crisis hit, there was a big reduction in linkage and, for the youngest workers, those under the age of 35, the linkage rate didn’t rebound,
said Mustard.
Something changed around this time in the reporting of work-related injury and illness to the Ontario WSIB,
he added. A plausible explanation for that would not be related to the discretion of the worker, but to the employment relationships that younger workers are in—perhaps more temporary employment, more gig work, and less standard employment through that time period.
Mustard noted that the method used in this study—linking two datasets that are population-based and have broad coverage—has strong potential to improve the reliability and validity of data on the health of Ontario workers. It allows policy-makers and other system stakeholders to look beyond workers’ compensation data as the main source of occupational health surveillance. It also allows for a deeper understanding of patterns of reporting and under-reporting. This information can be valuable in the targeting of labour inspection activity and may be useful in the design and delivery of worker awareness and training services,
he added.