Although death rates have fallen across all socioeconomic groups in Canada, inequalities in premature mortality—or death below the age of 75—have widened between people with the highest and lowest earnings and education levels over the period between 1991 and 2016, a new study has found.
The study was authored by Dr. Faraz Vahid Shahidi, Institute for Work & Health (IWH) Mustard post-doctoral fellow, and published in September 2020 in the Canadian Medical Association Journal (doi:10.1503/cmaj.191723).
The study found that, in 1991, men in the group with the lowest income were 2.1 times more likely than men in the highest income group to die early; by 2016, that difference had widened to 2.8 times more likely.
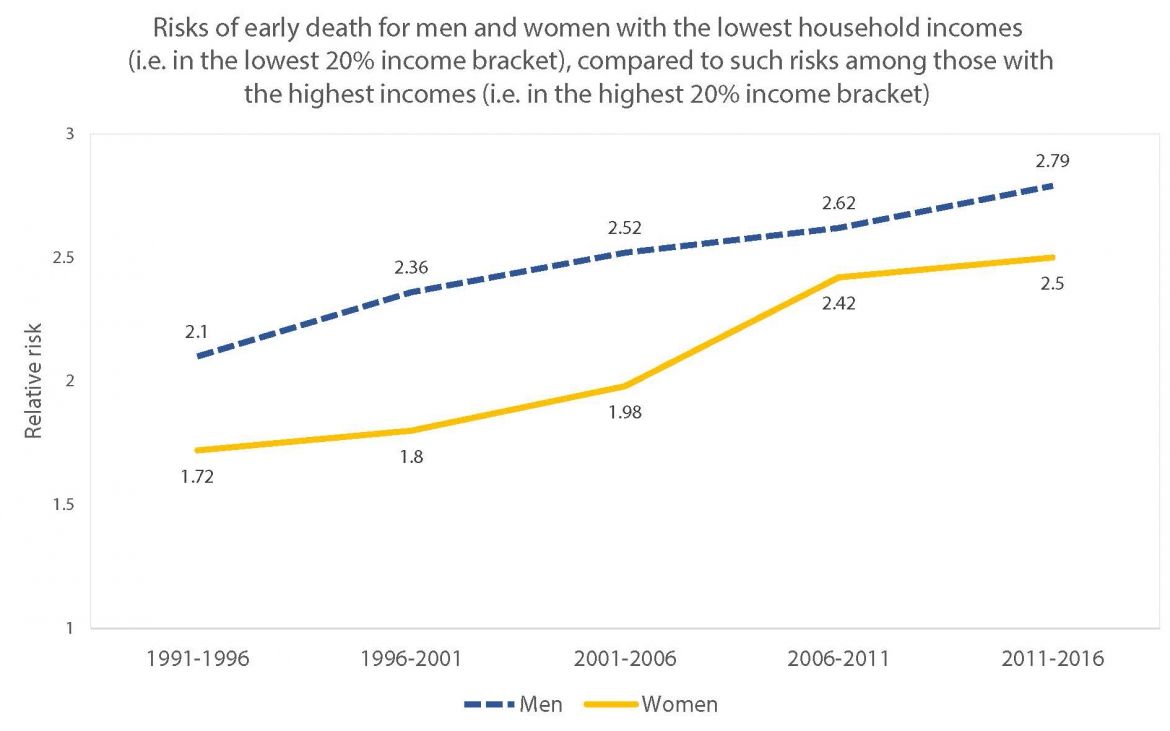
The widening gap was even more noticeable for women. In 1991, women with the lowest income had 1.7 times greater risk of premature mortality than women with the highest income; by 2016, that greater risk had grown to 2.5 times more likely.
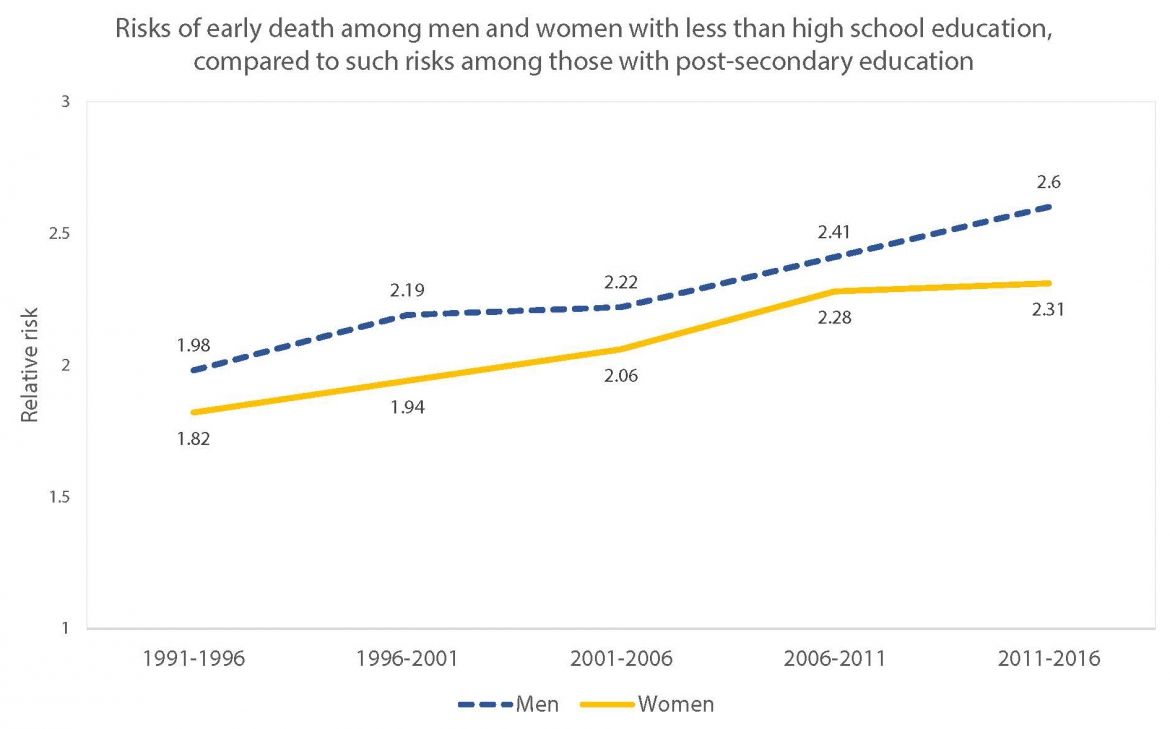
A similar pattern was found when it came to education levels. Among those without a high school degree, the risk of early death compared to those with a post-secondary degree increased from 2.0 to 2.6 for men and from 1.8 to 2.3 for women over the same 1991 to 2016 period.
The findings were not altogether surprising as similar patterns have been reported in the United States and many European countries, says Shahidi.
“Within the context of declining overall mortality rates, what we asked was, are gains in years lived accruing to some socioeconomic groups more than others?” says Shahidi. “If we believe that health equity is a moral good and a policy priority, then we ought to document whether progress has been made towards reducing mortality inequalities over the last few decades. On balance, our findings suggest that we have made little progress.”
Inequalities growing
Shahidi’s team conducted the study using a data linkage between the Canadian Mortality Database and five cycles of Statistics Canada’s Canadian Census Health and Environment Cohorts (1991, 1996, 2001, 2006 and 2011). The team focused on early deaths, as opposed to all deaths, in order to avoid what’s called “survivorship bias.”
“The term ‘survivorship bias’ refers to the general finding that people who survive into older adulthood represent a highly selected group of healthy individuals. This type of selection is particularly strong at the lower end of the socioeconomic spectrum and can therefore lessen the extent of health inequalities observed among the oldest age groups,” says Shahidi.
In their analysis, the team examined differences in death rates across four groups broken down by levels of education (less than a high school degree, a high school degree, some post-secondary education and a post-secondary degree) and five groups broken down into quintiles (i.e. 20 percentiles) based on household income.
In absolute terms, the team saw inequalities narrow between higher and lower income men but widen between higher and lower income women. Gaps across levels of education also widened for both men and women. The difference in early death rates between people with a post-secondary degree and people with no high school degree increased: from 792 deaths per 100,000 in 1991 to 1,119 per 100,000 in 2011 for women and from 1,713 per 100,000 in 1991 to 1,843 per 100,000 in 2011 for men.
The educational differences are starker, Shahidi explains, because of rising levels of education in the population during that time. “To lack a high school diploma today means something very different from what it meant in 1991. On average, it’s a much more severe marker of disadvantage now than it was 30 years ago.”
Indeed, Shahidi notes, for those with less than high school education—who made up 35 per cent of the sample in 1991 but only 14 per cent of the sample in 2011—absolute mortality rates stagnated among men and rose among women. “It’s bad enough that we see stagnation in the last decade and a half among men. Even more concerning, however, is the rise in premature mortality observed among socioeconomically disadvantaged women,” says Shahidi.
He adds that these adverse trends are likely related to broader societal trends occurring at the time, including rising levels of income inequality and declining social safety nets.