The fall of 2020 was a challenging time for those in Ontario's school system. Having made an emergency pivot to a virtual format the previous spring, students, families and educators entered a new school year with a sense of uncertainty—about infection risks that still remained, changes to the learning environment, and further disruptions potentially still ahead.
New classroom routines included masking, cohorting, staggering recesses and lunch breaks, posting lessons online in anticipation of student absences and school closures, and more.
A pair of peer-reviewed papers by the Institute for Work & Health (IWH) and Occupational Health Clinics for Ontario Workers (OHCOW) now paints a picture of the toll taken on Ontario educators from November to December 2020.
The two papers highlight the psychological strain educators were under during that unusual time,
says John Oudyk, an occupational hygienist at OHCOW and co-author of the papers. The ones who worked or taught in a virtual environment felt isolated and unsupported, while those who taught in person experienced anxiety related to the risk of COVID transmission.
In-person vs. online work
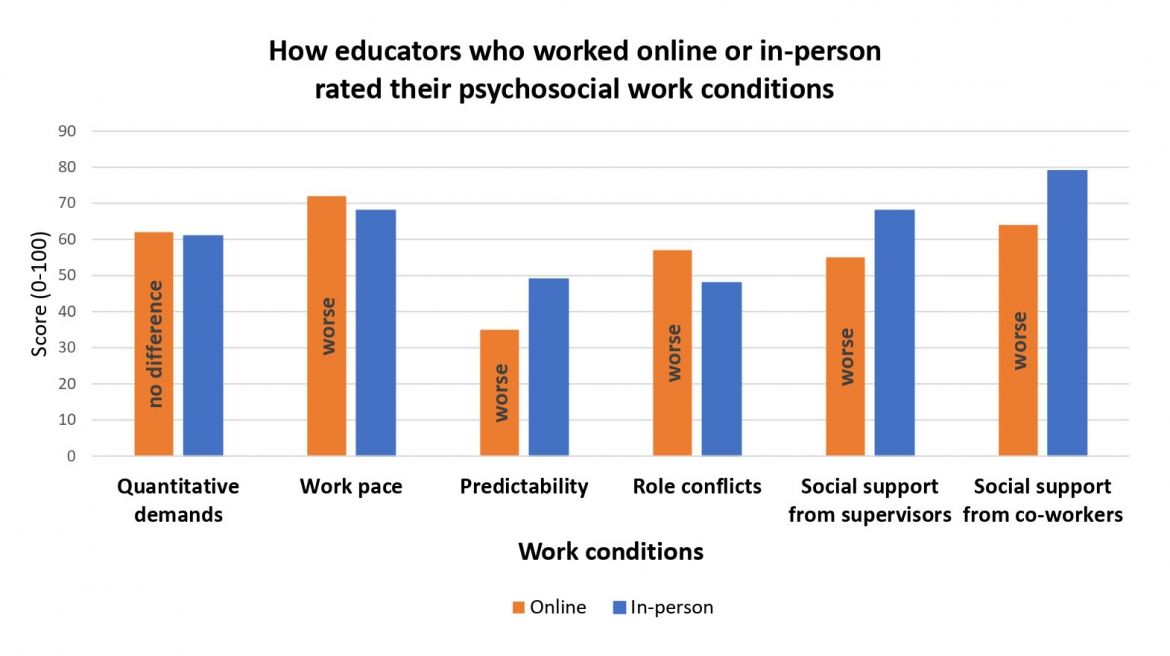
The first of the papers compared the experiences of in-person educators with those of virtual ones. The open-access paper, published in June 2022 in Occupational Medicine (doi:10.1093/occmed/kqac050), found educators who taught virtually had poorer psychosocial work conditions than in-person teachers across several areas.
Those working virtually had higher work pace, lower supervisor and co-worker support, greater role conflict, and lower job predictability than in-person teachers. Virtual teachers also reported more burnout symptoms than in-person teachers, but were no different in how many symptoms of poor sleep they experienced. Virtual educators and in-person educators also had similar scores for quantitative work demands.
One of the key things we found was that many of the scores related to psychosocial working conditions were worse for educators working online, compared to those working in-person,
says Dr. Peter Smith, IWH president and senior scientist and a co-author on the study.
Having vs. lacking COVID protections
The second of the two papers, which was published in November 2022 in the Journal of Occupational and Environmental Medicine (doi:10.1097/JOM.0000000000002693), examined the extent to which educators who physically went to work felt they had adequate protection from COVID transmission. It found two-thirds (66.5 per cent) said less than half of needed infection control protocols (ICPs) were in place. It also found this group—the ones who felt less protected—were three times more likely to have moderate or severe anxiety than those who said they had all the protections they needed.
In the study, the infection control practices most reported to be lacking included physical barriers, physical distancing from students, screening of students and visitors, cohorting of students, and masking requirements of students.
The study also asked whether participants had the personal protective equipment (PPE) they needed. About one in six (17.5 per cent) of those surveyed said half of their PPE needs were unmet. Among this group—the ones who reported inadequate PPE—the likelihood of experiencing moderate or severe anxiety was about 40 per cent higher than among those who felt all their PPE needs were met.
Examples of unmet PPE needs included lack of eye protection, N95 masks, face shields, and soap and running water. Notably, the lack of soap and running water was reported by one in four study participants.
Although the results showed a relatively high level of PPE implementation, prevention practices that were harder to implement were less in place, says Smith. If we consider changes in how workers performed their duties, administrative controls to increase distancing or other engineering controls, these appeared to be less well addressed. But many would argue that addressing these higher-level controls is more effective than worker-level controls like PPE,
he adds.
The study reinforces the importance of health and safety, not only in preventing work-related illnesses and injuries but also in safeguarding workers’ mental health. We can only assume those workers who felt protected were probably at lower risk of COVID transmission (as we didn’t measure this),
says Smith. But we do know that when workers felt protected, they reported fewer symptoms of anxiety. So ensuring workers have adequate protection when hazards are present (in this case, COVID risks) can bring benefits for both worker physical and mental health.
Questions from a teachers' union
Both papers drew on a survey developed by OHCOW in collaboration with the Elementary Teachers Federation of Ontario (ETFO). The educators’ union had approached OHCOW to survey its membership because it wanted to know what members were experiencing; how well personal protective equipment and infection control practices were working; and what impact online teaching had on members’ psychosocial work conditions.
The survey asked members to rate their psychosocial work environment using a short version of the Copenhagen Psychosocial Questionnaire (COPSOQ), a measure that had been previously validated among Canadian workers. The first paper was based on these survey responses.
The survey also asked educators about the extent to which needed PPE and infection control protocols were in place, and about their mental health via a widely used anxiety clinical screening tool (the Generalized Anxiety Disorder questionnaire or GAD-7). These survey questions drew on a design that had been developed by OHCOW and used earlier in the pandemic (once in a study of health-care workers and again in a study of the general worker population, with IWH providing conceptual and analytical support for both). The second paper was based on these survey results.
The survey was administered to ETFO members in November and December 2020, a time when the province’s second wave was continuing to build (ultimately leading to a week of extended virtual learning for all schools after the winter break, followed by partial reopenings at different public health units through mid-February 2021).
Of the 5,438 who took the survey and were working regularly at the time, the vast majority (87 per cent) delivered in-person teaching at a school worksite. Of the study participants who taught virtually, 68 per cent worked from home and 29 per cent delivered online lessons from a school site.
Smith points to this collaboration between IWH and OHCOW as a good example of the province’s health and safety system partners working together. The project began with a set of questions from a stakeholder group, the ETFO. It benefited from OHCOW working with ETFO and IWH on the design of the survey and working with the ETFO on recruiting educators to respond to the questions. Our main contribution, in turn, included ensuring the scientific analyses were conducted rigorously and independently, and guiding the work through the peer-review process,
says Smith. Together, we were able to arrive at a better understanding of the experiences of an important group working on the frontlines during the pandemic.